 (212) 861-9797
(212) 861-9797
 (212) 861-9797
(212) 861-9797
Macular pucker is a name given to a condition in which scar tissue grows in appropriately over the surface of the macula. This same condition has been called cellophane retinopathy, macular wrinkle, and epiretinal membrane. A jelly-like substance called the vitreous fills the central portion of the eye. It is composed of 99% water, some chemicals to create the gel, and long protein fibers. As we age the vitreous begins to shrink. The jelly starts to break down and the protein fibers start to aggregate.
In most people the vitreous eventually separates from the retina in a process called posterior vitreous detachment. In about 6% of people the detachment of the vitreous causes a wound healing response. The separation of the vitreous doesn’t seem like a traumatic event, but in some people their eye grows a fine layer of scar tissue over the macula, which is the portion of the retina in the back of the eye that has good visual acuity.
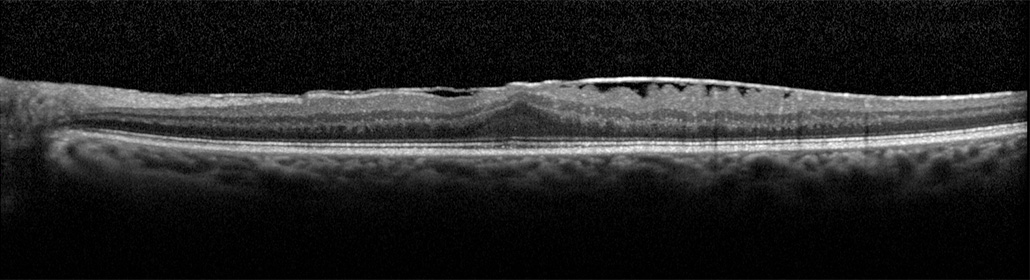
The scar tissue grows for a short period of time – usually a few weeks at most. Similar to what it does elsewhere in the body, scar tissue then begins to shrink. This causes the macula to wrinkle. If a thread in a piece of fabric is pulled the fabric will also wrinkle. This is how the term macular pucker was derived. The thin sheet of scar tissue is light gray and reflective, and when it gets wrinkled it looks like crumbled cellophane, thus the term cellophane maculopathy. The scar tissue can affect how the light rays course to the retina, the retina itself is crumbled by the scar tissue, and secondarily the macular may become swollen.
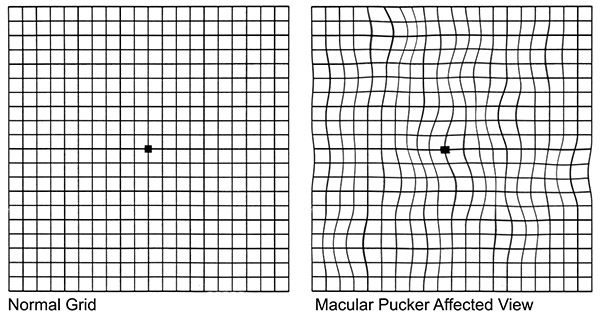
All of these factors cause the vision to become decreased and distorted. Chronic deformation of the macula by the scar tissue can cause cumulative damage, with slowly decreasing visual acuity in some patients. Fortunately in most patients the visual acuity generally remains stable.
 The symptoms for macular pucker are also common to other conditions that affect the macula. They include:
The symptoms for macular pucker are also common to other conditions that affect the macula. They include:
1. Distortion to letters and lines when reading.
2. Decrease in central vision for both distance and near vision.
3. Difficulty reading or carrying out tasks that call for fine visual detail.
I just love Dr. Klancnick. He is caring, but more than that, he has taken the fear out of going to my Retina doctor. I now get injections directly into my eye, and needless to say this is a scary experience. Dr. Klancnick explains everything to me about the procedure and shows me my improvement. I was so lucky to find him when I moved back to Brooklyn. As I praise him, I must also praise his kind and professional staff. They are great!!!
JODI B Google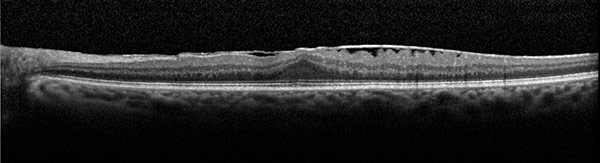
The doctors at VRM will by examining the macula. The most important test following direct examination is optical coherence tomography. This imaging method provides highly detailed cross-section information of the macula. It enables the doctors at VRM to assess the scar tissue and the effects on the macula.
Color photography of the macula is helpful in documenting the extent of the scar tissue. On occasion fluorescein angiography is done to determine if the eye also has macular degeneration in addition to the pucker.
 The treatment options for macular pucker depend on the severity of the condition and the individual’s visual symptoms. If you are not that bothered by the decrease in vision or the distortion, then surgery for macular pucker is usually not indicated. We generally don’t want to operate on patients unless they are unhappy with their vision. If your vision is decreased or distorted enough that you are not happy or you can’t perform occupational tasks, macular pucker surgery may be indicated.
The treatment options for macular pucker depend on the severity of the condition and the individual’s visual symptoms. If you are not that bothered by the decrease in vision or the distortion, then surgery for macular pucker is usually not indicated. We generally don’t want to operate on patients unless they are unhappy with their vision. If your vision is decreased or distorted enough that you are not happy or you can’t perform occupational tasks, macular pucker surgery may be indicated.
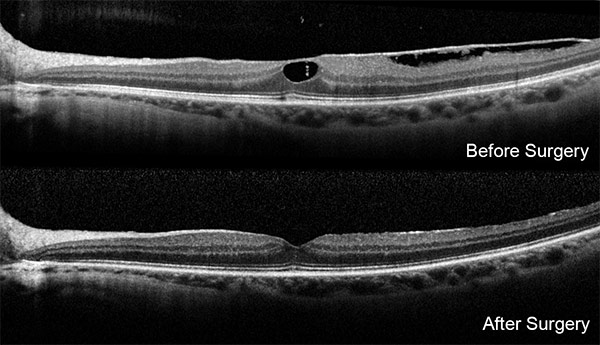
In many instances, macular pucker treatment is unnecessary because the distortion to vision is minimal. When vision loss is more pronounced, however, surgical repair may be necessary. Minimally invasive vitrectomy surgery is performed by doctors at VRM to remove the vitreous gel and then the doctors peel off the scar tissue. The scar tissue can be surprisingly tough skin on the surface of the macula. The underlying retina is often molded by the chronic distortion caused by the scar tissue and to allow the retina to relax to a greater extent an additional layer, the internal limiting membrane may be peeled as well.
Generally the patient uses eye drops for 2 to 3 weeks after surgery. Complications of the macular pucker eye surgery include an approximately 1% chance of causing a retinal tear or detachment that would require additional surgery to repair.
There is about a 1 in 2,000 to 3,000 chance of getting an infection in the eye, which would require antibiotics for treatment. Vitrectomy surgery causes cataracts to form sooner in life, probably because of increased oxygen delivery to the lens. The outside part of the eye looks normal within a couple of weeks but the vision may take months to reach its final level. The longer the scar tissue was present before surgery the longer it takes to reach the final improved acuity.
Most patients with macular pucker surgery improve by about 3 lines of visual acuity. A more complete description of what to expect, the possible complications, and how to use medications after surgery will be related to you by your retina doctors at VRM.
The doctors at VRM have a long history of developing the latest techniques in imaging macular pucker and their associated damage and surgery of macular pucker and related conditions. The scientific articles concerning the developments by VRM doctors can be found at the website of the National Library of Medicine.
Top-Quality Eye Care. Our New York ophthalmologists and eye doctors publish more in the foremost peer-reviewed journals about macular pucker treatments than any other private or academic group in the United States. Many current concepts in retinal disease and some of the best treatments recognized worldwide were invented at VRMNY ophthalmology center.
Groundbreaking Research. Our renowned retinal specialists lecture worldwide on retinal vascular disease and serve as academic leaders in the field as the most published group in foremost peer-reviewed journals in the U.S.
Reputation. Our reputation for outstanding eye care gives you access to the latest treatments and technologies and the best eye doctors to treat macular pucker. Our specialists authored numerous peer-reviewed journal articles and book chapters and has presented at scientific meetings nationally and internationally, and have been selected as Castle Connolly Top Doctors, New York Super Doctors, the prestigious group of New York Magazine Best Doctors.
Let us help you enjoy your life
Call: (212) 861-9797To Speak With An Appointment Coordinator Now