 (212) 861-9797
(212) 861-9797
 (212) 861-9797
(212) 861-9797

Many people with macular degeneration experience minimal vision loss during the early stages of the disease. For most people, macular degeneration does not become vision impairing. During this stage, the transport of wastes and nutrients by the RPE has slowed down. As a result, waste builds up under the retina and forms yellowish deposits known as drusen.
An ophthalmologist examining a patient at this stage may see drusen, although no symptoms may be present or develop later. If the doctor sees drusen, the patient will be monitored. In most cases, the disease will not progress to vision loss, although some patients do experience vision loss with drusen. Many patients over 60 have some drusen.
There are two types of AMD:
Macular degeneration may progress into dry (atrophic) macular degeneration or wet (exudative) macular degeneration.
Dry macular degeneration generally progresses slowly as drusen accumulate in the retina. This condition rarely leads to severe vision problems or blindness. While portions of the RPE continue to slowly transport wastes and nutrients, photoreceptors accrue damage over time. The number and size of drusen increase in the macula.
Visual changes often correlate with the loss of function of the corresponding areas of the retina. Sometimes large regions of cells are lost. This is known as geographic atrophy. Geographic atrophy may cause a blind spot or scotoma in the central vision.
If you have dry macular degeneration, you should tell your ophthalmologist about any changes in your vision immediately. Regular exams along with self-monitoring using the Amsler Grid or other devices are necessary for preserving your vision. Patients with dry macular degeneration can develop wet macular degeneration, for which effective treatment is available if instituted in a timely manner.
Aside from managing your risk factors and vitamin therapy, there is currently no other prevention or treatment for dry macular degeneration. Luckily, most people with dry macular degeneration do not progress to more advanced geographic atrophy or the wet form. Preventing dry macular degeneration or halting its progression are areas of intense research. VRMNY is actively participating in promising trials dedicated to this endeavor.
People with large drusen, many drusen that run together, or focal pigmentation are more likely to develop wet macular degeneration. With this form of the disease, new abnormal blood vessels grow under the retinal pigment epithelium, under the retina, or even within the retina. These new blood vessels originate in the context of choroidal neovascularization (CNV).
It is believed that these new blood vessels form in response to impaired retinal nutrient supply and the slowed transport of wastes. New blood vessels often leak blood or fluid under or into the retina. As this happens, the surface of the retina becomes uneven, thus objects in that part of the vision field may appear distorted, wavy, or blurry. The new blood vessels may break through some of the retinal layers. If parts of the retina become damaged by these blood vessels, it may cause blind spots.
In most cases, the first sign of fluid under the retina is the appearance of distorted straight lines. Regular testing with an Amsler Grid can be helpful in detecting problems early. If detected early, new blood vessels can be treated before they cause too much damage. Ultimately, untreated neovascularization and leakage can cause the overlying photoreceptors to die and macular scarring. The final stage of macular degeneration is scarring, which in most cases leads to vision loss.
Macular degeneration only affects central vision, and although it is the leading cause of legal blindness, it rarely causes total blindness. In other words, even patients with very advanced stages of the disease are able to navigate their homes and neighborhoods and will not have to depend on guide dogs or other aids that are commonly associated with total blindness.
From the moment you enter the office you are treated with respect from all the staff. The office operates efficiently to ensure that all patients have the time to be seen and talk with their physicians. I am very pleased with the care. Compassion and overall kindness that has been shown to me.
Margaret M. Google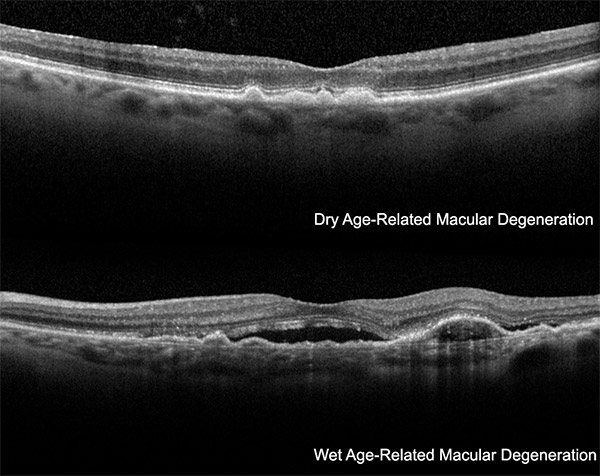 An ophthalmologist can identify macular degeneration or determine if you are at risk for developing the disease. Your exam will begin with a test to measure the sharpness of your vision. The most common visual acuity test features lines of black letters on a white chart. Next, your doctor will determine if you have areas of reduced or distorted vision using an Amsler grid. Reduced and distorted vision are common symptoms of macular degeneration.
An ophthalmologist can identify macular degeneration or determine if you are at risk for developing the disease. Your exam will begin with a test to measure the sharpness of your vision. The most common visual acuity test features lines of black letters on a white chart. Next, your doctor will determine if you have areas of reduced or distorted vision using an Amsler grid. Reduced and distorted vision are common symptoms of macular degeneration.
After these tests, the ophthalmologist will evaluate the front of your eyes and measure eye pressure. Next, your retina will be examined using a special microscope known as a slit lamp. Your pupils will need to be dilated for a thorough exam. Using the slit lamp, the ophthalmologist can check for drusen, atrophic areas, pigmentation, and identify any other retinal abnormalities.
Early choroidal neovascularization is typically not visible, but the ophthalmologist can look for symptoms that indicate it, including bleeding or fluid behind or within the retina. In this case, more testing is needed.
 While there is no cure for AMD, the doctors at Vitreous Retina Macula Consultants of New York offer advanced treatments that stabilize the progression of the disease and, in some cases, improve vision. Our specialists help preserve eyesight for people with age-related macular degeneration through early diagnosis and expert care.
While there is no cure for AMD, the doctors at Vitreous Retina Macula Consultants of New York offer advanced treatments that stabilize the progression of the disease and, in some cases, improve vision. Our specialists help preserve eyesight for people with age-related macular degeneration through early diagnosis and expert care.
Over the last 10 years, wet AMD has seen a revolution in treatment modalities and patient outcomes. Injection therapy with a variety of agents has become the mainstay of therapy and enabled us to provide patients with unprecedented visual acuity gains and disease stability for many years. More potentially destructive therapies like “hot” and “cold laser” are now only used in a minority of cases where these modalities are appropriate.
Anti-VEGF Medications
Vascular endothelial growth factor (VEGF) is a substance produced by the body to regulate the growth and health of blood vessels. In wet AMD, an excess of VEGF leads to formation of new, unhealthy blood vessels. Several drugs are available to block VEGF and help control wet AMD. They all need to be injected into the eye through the white part with small needles that create a self-sealing entry site.
These injections need to be carried out with a certain regularity to improve and then maintain visual acuity. Often times, three initial monthly injections will be performed, followed by more stretched out intervals between injections. Unfortunately, only a few patients with wet AMD get away with infrequent injections or stopping injections altogether. Luckily, the injections are not as uncomfortable as one may imagine and even the rare patients who need monthly injections in both eyes do tolerate this very well.
At VRMNY, patients with Macular Degeneration are offered all possible medication options to provide you with the best outcome in your particular situation.
VABYSMO (Faricimab-Svoa)
Vabysmo was approved by the FDA in 2022. When compared with Eylea, it appeared to last longer, while providing the same vision gains. Side effects appear to be similar to Lucentis and Eylea.
Macugen
Macugen was the first drug approved to treat wet AMD. Macugen appears to be much less effective than the other anti-VEGF medications and is therefore only rarely used nowadays.
Lucentis
Lucentis was the second drug to be approved by the FDA for the treatment of wet AMD. Its effect is more powerful than Macugen’s. On average, 21 letters on a specialized reading chart (ETDRS chart) were gained, and about 40 percent of patients regained the ability to read newspaper print (20/40). Not all patients did improve their vision, but 90 percent resulted better or stable vision.
These results of the wet macular degeneration treatment using Lucentis represented a breakthrough compared to the natural history of the disease, which essentially leads to legal blindness in the vast majority of patients.
Eylea
Eylea is the most recent addition to the drug armamentarium against wet AMD. Visual results comparing Lucentis and Eylea appear to be equivalent. For some patients, one drug may work better than the other, so VRMNY physicians will sometimes switch between the two to provide you with the best possible outcome to treat wet macular degeneration.
Avastin
Prior to the approval of Lucentis, doctors were using a related drug called Avastin. Avastin produces similar results as Lucentis, as recently demonstrated in a large study sponsored by the National Eye Institute. Lucentis and Eylea are about $2000, while Avastin is only about $50. Both drugs are covered by insurance plans for the treatment of wet AMD. Our staff will help you apply for copay assistance, should you not have a secondary insurance.
So far, only Lucentis and Eylea have been approved for treating wet AMD. Avastin eye injections for macular degeneration are prepared by a compounding pharmacy rather than the manufacturer itself, therefore introducing another potential step for contamination, which could lead to an infection after the injection. Your doctor will discuss the risks, benefits, and alternatives of these medications with you to make the right decision based on your individual situation.
Visudyne Photodynamic Therapy/Cold Laser Treatment
Photodynamic, or “cold laser” therapy has been used to treat some cases of wet macular degeneration since 2000. With this treatment, leaking blood vessels in the retina are destroyed using a laser and a light sensitive drug that is administered into a vein in the arm. Within the bloodstream, this drug attaches itself to low-density lipoprotein (LDL). In the retina, abnormal blood vessels attract and absorb LDL.
During the procedure, the eye is numbed and a contact lens is placed over the eye to focus the laser. Then, laser energy is transmitted to the area of choroidal neovascularization. Laser energy stimulates the drug within the abnormal blood vessels, closes them, and causes them to stop growing. The procedure itself does not damage the retina. In some cases, your ophthalmologist may inject a steroid in the affected eye to reduce swelling and inflammation.
The whole procedure typically lasts less than 30 minutes. Afterward and for the next five days, you should not expose yourself to direct sunlight or other bright lights as the drug is cleared from your body.
Generally, several sessions of photodynamic therapy are required to treat wet macular degeneration. Commonly, patients have three to four treatments the first year and two treatments the next year. Your doctor can use OCT imaging or an angiogram to decide if more treatment is needed.
Argon Laser Photocoagulation/Hot Laser Treatment
Another type of treatment for wet macular degeneration utilizes a thermal laser to clot the areas of choroidal neovascularization and prevent spreading.
Laser treatment is usually done on an outpatient basis using anesthetic eye drops. During the procedure, your ophthalmologist utilizes a slit lamp to get a magnified view of the retina. Then, the laser is pointed directly at the choroidal neovascularization beneath the retina. Minimal discomfort is to be expected.
As laser light passes through the retinal tissues, it is absorbed by the choroidal neovascularization and the RPE and choroid. This absorption produces heat, which burns the choroidal neovascularization as well as some surrounding retinal tissues. This causes a small scar to develop. Following treatment, the scarred area appears as a permanent blind spot.
Laser treatment usually does not improve vision. A small part of the retina has to be sacrificed to avoid more extensive damage. The scar caused by the laser is much smaller than if the choroidal neovascularization were not treated. Currently, this treatment is reserved for lesions that are far away from the visual center.
Risk factors for developing macular degeneration include:
Several studies have been conducted to see if antioxidant supplements can prevent or slow the advancement of macular degeneration. A series of important studies, the Age-Related Eye Disease studies conducted by the National Eye Institute, showed that a defined subgroup of patients with macular degeneration who were at risk for developing an advanced form of AMD benefitted from taking supplements with zinc and antioxidants as well as lutein and zeaxanthin. Patients with AMD should discuss the findings of this study with their ophthalmologist to see how it applies to their condition. It is important to determine whether these supplements are right for you, since they are not free of potentially serious side effects.
Research indicates that patients who eat a lot of spinach and collard greens are less likely to develop macular degeneration. Spinach, collard greens, and other green leafy vegetables are good sources of lutein and zeaxanthin, two important macular pigments. These nutrients are also found in yellow corn, broccoli, oranges, avocados, and egg yolks.
Some people with macular degeneration lack the mineral zinc, which can be found in meat, fish, beans, pasta, oats, and shellfish.
Studies indicate that patients with a high concentration of omega-3 fatty acids in their diet are less likely to develop macular degeneration. Omega-3 fatty acids may also prevent damage to the retina. Fish, fish oils, walnuts, and certain plant oils are good sources of omega-3 fatty acids.
We recommend you eat a balanced diet with fruits and vegetables and limit excessive saturated fats and cholesterol. Talk with your ophthalmologist about the benefits of taking a multivitamin or antioxidant supplement.
Schedule an appointment with an eye doctor if you have areas of reduced or distorted vision, can’t see clearly at a distance, have problems transitioning from dark to bright light, or need ever brighter light to read by.
Wet AMD damages the macula much more quickly, but with regular Amsler Grid testing, we can detect problems early so new blood vessels can be treated before they cause too much damage. Consult an eye doctor as soon as possible if you experience noticeable differences in your sight, such as blurry or distorted vision, as it could be a sign of macular degeneration scarring, which in most cases leads to vision loss.
Age-Related Macular Degeneration is worrisome for older people, but with proper diagnosis, the best eye doctors for macular degeneration at Vitreous Retina Macula Consultants of New York, will help you manage your condition and protect your vision.
Cutting-Edge Diagnostics.Early detection of age related macular degeneration (AMD) is crucial in order to preserve vision and the quality of life. New technologies we are using at VRMNY allow for earlier detection and vision preservation in AMD patients.
Newest Treatments.As leading experts in the treatment of Macular Degeneration, our retina doctors research and develop new diagnostic and therapeutic strategies. Many current concepts in diagnosing and treating Age-Related Macular Degeneration recognized worldwide were invented at the VRMNY.
World-class specialists.Our renowned retinal specialists lecture worldwide on macular degeneration (AMD) and serve as academic leaders in the field as the most published group in foremost peer-reviewed journals in the U.S.
Reputation.Our reputation for outstanding eye care gives you access to the latest treatments and technologies and the best eye doctors for macular degeneration (AMD). Our specialists have been selected as Castle Connolly Top Doctors, New York Super Doctors, the prestigious group of New York Magazine Best Doctors, one of the best physicians in the United States by “The Best Doctors in America” and are consistently quoted by well-known retina specialists.
Let us help you enjoy your life
Call: (212) 861-9797To Speak With An Appointment Coordinator Now