 (212) 861-9797
(212) 861-9797
 (212) 861-9797
(212) 861-9797
The macula is the very small area in the back of the retina that is responsible for providing sharpness and clarity in our vision. This detailed vision is necessary for daily tasks such as reading, driving, and watching television. A jelly-like substance called the vitreous fills the central portion of the eye.
It is composed of 99% water, some chemicals to create the gel, and long protein fibers. As we age the vitreous begins to shrink. The jelly starts to break down and the protein fibers start to aggregate. In most people the vitreous eventually separates from the retina in a process called posterior vitreous detachment.
In some people the vitreous may remain adherent to the central portion of the macula and pulling by the vitreous can cause bad things to happen to the macula. Chronic pulling, or traction, on the macula can cause the macula to become distorted or stretched. In some people the force of the traction exceeds the mechanical strength of the macula and a hole can form.
Macular holes are typically very small – smaller in diameter than a pin. However the macula is very important for sharp vision and even a very small hole can cause important visual problems. The vision is generally decreased and distorted.
The curious aspect of macular holes is that they don’t heal themselves. If someone had their ears pierced, but didn’t wear an earring the hole would close. Only the smallest macular holes can close without surgery and even then the chance is low. The retina is really a type of brain tissue, and brain tissue doesn’t heal well. The steps naturally taken by the body to heal a macular hole can make it get larger over time.
 The most common symptoms for a macular hole include:
The most common symptoms for a macular hole include:
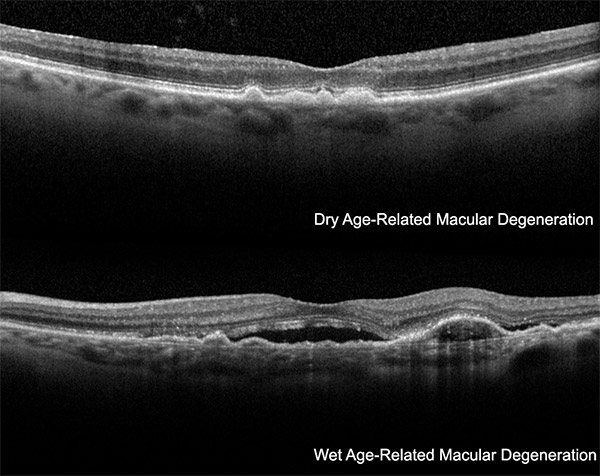
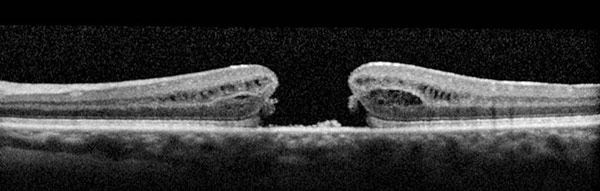 Doctors at VRM diagnose a macular hole by first looking into the eye. Important characteristics of a macular hole can be determined from measurements made from color photography or by evaluating images obtained by optical coherence tomography.
Doctors at VRM diagnose a macular hole by first looking into the eye. Important characteristics of a macular hole can be determined from measurements made from color photography or by evaluating images obtained by optical coherence tomography.
These evaluations are done in our office using a special computer system that allows the patient to see the images every step of the way. The three most important factors related to macular holes in increasing order of importance are the nature of the traction by the vitreous, the amount of scar tissue around the hole, and the size of the hole.
Continued traction to the hole alters the surgical approach somewhat. In trying to heal the hole, the body appears to make scar tissue that grows out of the retina at the edges of the hole. This scar tissue grows up and onto the retina. Scar tissue eventually shrinks, and this scar tissue enlarges the macular hole.
During the macular hole repair surgery, the scar tissue generally needs to be removed. The most important feature, by far, is the size of the hole. Very small holes may heal without surgical intervention, but over time most will get larger. On the other end of the spectrum large macular holes have a poor chance of closing even with surgery. These holes typically have been present for a long time.
 Macular holes are repaired by a set of techniques commonly referred to as “vitrectomy”. The goals of this surgery are similar to other types of tissue problems in the body. The jelly like substance is removed from the eye to gain access to the macula.
Macular holes are repaired by a set of techniques commonly referred to as “vitrectomy”. The goals of this surgery are similar to other types of tissue problems in the body. The jelly like substance is removed from the eye to gain access to the macula.
The structures leading to forces causing the hole to expand are removed, and the tissue is immobilized to help healing. If you break your arm, the doctor would put the bones back into proper position and then immobilize the bones by using a cast. While immobilized the bones heal. If you cut your arm the doctor would sew the skin back to- gether. This puts the skin back into proper position and immobilizes the skin so that it can heal.
The macular is a special tissue that poses difficult surgical challenges. The cells in the macula are very delicate. We can’t sew the macula together, because this would damage the light sensitive cells. Also there is no suture method that is small enough. We can’t use lasers, because lasers burn tissue, which would hurt the light sensitive cells.
Glues have the potential to stimulate scar tissue. So the surgical option we are left with is to remove the tissues and forces causing the hole to remain open and to immobilize the tissue, just as in other places in the body. We can’t use a cast for the retina, so instead we fill the eye with gas. The surface tension of the gas bubble immobilizes the hole.
With the retinal tissue in its proper position and immobilized, we hope the hole will close. The amazing thing is that it often does close. Small holes close a little more than 90% of the time after 1 operation. Once the hole size exceeds 400 microns in diameter – about the equivalent thickness of 4 pieces of paper stacked together – the proportion of successful cases drops off dramatically.
Back in the old days (the 1990s) this involved making relatively large incisions in the eye. The scar tissue and related layers were sometimes removed, sometimes not, and a gas bubble that lasted up to 6 weeks was used. During that time the patient had to keep their face down, top position the gas bubble over the hole.
Dr. Engelbert has gone above and beyond every appointment! The most thorough and well educated eye Dr. I’ve seen out of many… Very patient and answers all questions for the best plan of care. Thank you!
With more modern advances in surgery, everything has changed. The incisions are very small and constructed in a way that sutures are not commonly used. The need for head down position has changed as well. It is common for patients to keep their face down for only a few days, although the size of the hole and other factors are considered when the actual recommendations for macular hole surgery are made by VRM doctors.
Generally the patient uses eye drops for 2 to 3 weeks after the macular hole repair surgery. Complications of the surgery include an approximately 1% chance of causing a retinal tear or detachment that would require additional surgery to repair. There is about a 1 in 2,000 to 3,000 chance of getting an infection in the eye, which would require antibiotics for treatment.
Vitrectomy surgery causes cataracts to form sooner in life, probably because of increased oxygen delivery to the lens. The outside part of the eye looks normal within a couple of weeks but the vision may take months to reach its final level. Most patients with macular hole surgery improve by about 3 lines of visual acuity. A more complete description of what to expect during the surgery for macular hole, the possible complications, and how to use medications after surgery will be related to you by your doctor at VRM.
At Vitreous Retina Macula Consultants of New York, one of our ophthalmologists and retina specialists will meet with you during your consultation to assess your situation. We will explain each treatment option’s pros and cons and suggest which treatment to repair a macular hole is right for you. VRMNY eye surgery center in New York specializes in treating all medical and surgical retinal conditions, emphasizing Vitreomacular Traction and Macular Hole. Request an appointment online or call the internationally-renowned retina specialists and best-rated Macular Hole Doctors at (212) 861-9797 to schedule your private consultation.
Latest Techniques. The retina doctors at VRM have a long history of developing the latest techniques in imaging macular holes and their associated damage, devising the theory of macular hole development, and surgery of macular holes and related conditions. The scientific articles concerning the developments by VRM doctors can be found at the website of the National Library of Medicine.
Groundbreaking Research. Our physicians first developed a practical method to image deeper structures in the eye with optical coherence tomography. Our renowned retinal specialists lecture worldwide on retinal vascular disease and serve as academic leaders in the field as the most published group in foremost peer-reviewed journals in the U.S.
Technologies. Our doctors utilize all forms of ophthalmic imaging, including fluorescein angiography, indocyanine green angiography, and noninvasive forms of imaging such as spectral-domain optical coherence tomography, autofluorescence photography, and ultrasonography.
Leading Retina Doctors. The doctors at VRMNY authored and co-authored over 1000 articles in peer-reviewed journals and have lectured at many scientific meetings worldwide. Some of our experts are recipients of the Honor Award and have participated in many of the American Academy of Ophthalmology teaching activities.
Let us help you enjoy your life
Call: (212) 861-9797To Speak With An Appointment Coordinator Now