 (212) 861-9797
(212) 861-9797
 (212) 861-9797
(212) 861-9797
As nationally recognized experts, the best-in-class retina doctors at VRMNY can quickly pinpoint the cause of retinal detachment and develop a treatment plan that preserves the eye’s health. Our doctors are foremost experts in the treatment of retinal detachment, conduct research and develop novel diagnostic and therapeutic approaches. VRMNY provides laser procedures to repair a tear in the retina, stop a detachment, or keep a small detachment from growing larger. If the retinal detachment is severe, our doctors may advise surgery.
The retina can be likened to film in a camera. It is the light sensitive structure that lines the back of the eye. The part directly in the back of the eye is the macular region. Because of the structure of the macula and the cells that are there, the macula supplies sharp vision and also provides most of the color information being sent back to our brains.
The rest of the retina supplies a lower resolution image that gives us the wide field of view we ordinarily have. This side vision is very important in functioning in the modern world. The retina is not connected to the back of the eye in a firm way. Under some circumstances the retina can pull away from the back of the eye. Since the retina gets much of its oxygen and nutrition from the tissue in the back of the eye, this can lead to significant harm to vision.
There are many different ways the retina can detach from the back of the eye. One way is that it can be pulled by force. There is no hole or tear in the retina, just brute force. A second way is the retina can tear and fluid from the middle part of the eye can go under the retina; this method combines pulling with fluid flows to cause the retina to separate from the back of the eye. The third important way is there can be an excessive amount of fluid made under the retina by disease and the rising tide of fluid floats the retina away from the back of the eye.
Some diseases, such as diabetes, cause blood vessels and cells similar to those found in scar tissue to grow into the middle parts of the eye from the retina. At first these stalks look like treed or fans of seaweed. Eventually they contain more and more scar. Also since they contain blood vessels these fronds can also bleed. Bleeding commonly leads to more scar tissue. Contraction of the scar tissue can pull the retina away from the back of the eye. Many different conditions can lead to the same endpoint. In many patients the simple passage of time causes the vitreous to pull on the retina, at least a little. In some patients this pulling can be extreme and lead to detachment of the macula.
Excessive pulling, especially if concentrated to a small area, can cause the retina to tear. Fluid from the vitreous cavity can come in through the hole and accumulate under the retina. This type of retinal detachment has an excessively complicated name, a rhegmatogenous retinal detachment. Retinal tears leading to detachment is the most common form of retinal detachment leading to eye surgery. The link between retinal tears and detachments didn’t happen that long ago in medical history. There was no way to look into the eye until about 150 years ago. It took many years to develop methods that allowed examination of the entire retina. Once that happened people realized the retina could detach, and they saw the retina had tears, but thought the tears occurred because the retina was detached, not the other way around.
A complicated net of blood vessels exists under the retina in a structure called the choroid. The retina has the highest need for oxygen in the body per gram of tissue. If the retina had enough blood vessels to supply this requirement we would have a difficult time seeing because of all the blood vessels. Instead the eye has a nice design feature. A dense network of blood vessels delivers oxygen to the retina from below. This layer is called the choroid, and the choroid has the highest blood flow per gram of tissue in the body. Problems can arise if the vessels in the choroid become excessively leaky. If you have ever injured your elbow or knee you know the joint can become swollen. The swelling is from fluid leaking from blood vessels. Imagine the choroid – if that becomes inflamed there are many vessels that could leak. Fluid produced in the choroid will make that layer swollen, but the fluid oozes up under the retina and accumulates there. In exudative detachments the retina is floats off of the back of the eye.
 The most common symptoms include:
The most common symptoms include:
1. Decreased visual acuity
2. Dark regions in the field of vision
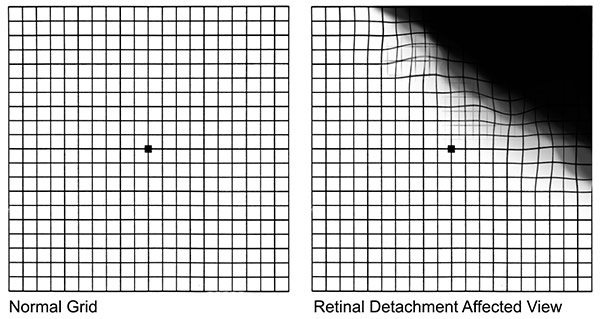
3. Distorted vision
 The principle way doctors at VRM diagnose a retinal detachment is through direct examination of the eye. This can help identify which of the three types of causes for retinal detachment is the problem. Additional testing is required to evaluate this initial hypothesis. Ultrasound is used to evaluate the position of the retina and to look at deeper structures in the eye.
The principle way doctors at VRM diagnose a retinal detachment is through direct examination of the eye. This can help identify which of the three types of causes for retinal detachment is the problem. Additional testing is required to evaluate this initial hypothesis. Ultrasound is used to evaluate the position of the retina and to look at deeper structures in the eye.
Optical coherence tomography provides cross-sectional information about the retina and choroid. Fluorescein angiography is very helpful in grading the amount of leakage in exudative detachments. As in other fields of medicine diagnostic testing helps establish the diagnosis, the mechanism of disease, serves to document disease severity, and helps in monitoring disease progression.
Considering the importance of vision and the numerous serious diseases which pose a life changing threat, there is no room for error. The finest eye specialists in the country are found at VRMCNY. I have been a patient there for decades and have been seen by several doctors. They define the meaning of expert and consult with one another to ensure accuracy. The office is spotless. The staff is courteous and professional. The visits are usually time consuming due to the necessity of imaging and a preliminary exam with a technician before seeing the specialist. I consider myself fortunate and am very grateful to be a patient there.
RENEE B. GoogleEach form of retinal detachment has a different cause, and to repair the detachment the root causes need to be addressed.
Once the source and extent of the traction is visualized, plans can be made to repair the same. In most cases of traction retinal detachment a vitrectomy is performed. This operation removes the vitreous, the jelly-like substance in the eye that typically provides the platform for the scar tissue to grow. In the process the tissue providing traction on the retina is also removed. Once the traction is removed there is no longer a reason for fluid to accumulate under the retina. However there is already fluid under the retina, since the retina is detached. To get the fluid out from under the retina a small hole is made in the retina and the fluid is sucked out. The small hole is covered with laser to weld the retina to the back of the eye. The eye typically is filled with gas to hold the retina in place until the laser weld strengthens.
A retinal tear leading to a detachment requires closing the retinal hole for the detachment to be repaired. When retinal doctors talk about closing a hole, what they mean is that the flow of fluid through the retinal tear to the space under the retina must be blocked.
There are 3 main ways to do this.
VITRECTOMY
The vitreous and any pulling by the vitreous is removed from the eye. The fluid under the retina is sucked out of the eye and laser welds are put around the tear to seal the tear so no new fluid can come under the retina. The eye is usually filled with gas to hold the retina in place until the weld s become strong. Sometimes a thick fluid, silicone oil, is used instead of gas.
The advantage of vitrectomy is the doctor can directly see the tear and the pulling and fix the problem. The disadvantage of vitrectomy is that the gas bubble used to hold the retina in place doesn’t work well if the defects in the retina are at the bottom of the eye because air bubbles rise. Patients can’t see well if their eye has gas. Cataracts are common after vitrectomy surgery. This type of eye surgery is generally done in a hospital setting.
SCLERAL BUCKLE
Instead of removing the traction, the wall of the eye can be moved toward the traction to relieve the force on the retina. To do this a piece of silicone is sewn on the outer wall of the eye. This can close many holes. A freezing probe can also be used to make welds between the retina and back wall of the eye.
The advantages of scleral buckles are they do not involve operating on the inside of the eye and broad areas of the retinal periphery can be supported by the buckle.
The disadvantages are the constant presence of a foreign body implanted in the eye, pain, double vision, and inability to repair certain forms of detachment. Scleral buckle eye surgery is generally done in a hospital setting.
PNEUMATIC RETINOPEXY
A gas bubble can be used to manipulate the position of the retina and to seal a tear in the retina, at least temporarily. In pneumatic retinopexy a gas bubble is put into the eye and the patient’s head is positioned to put the gas bubble over the tear. In many patients the fluid under the retina will be cleared by the body and laser welds will prevent any new fluid from coming through the tear. A freezing probe can also be used to make welds.
The advantages of pneumatic retinopexy are it a quick in-office procedure that is minimally invasive.
The disadvantages are not all types of retinal tears can be repaired and the proportion of success is lower than in other forms of retinal surgery.
Successively putting the retina back into place is common after surgery. The success rate of the retinal detachment surgery depends on the mix of cases examined in any one study, but for most studies the proportion is about 90%. Of the failures many can be eventually repaired with an additional surgery. The amount of visual acuity return after surgery depends on the amount of damage occurring before the surgery. Detachment of the macula leads to damage and a predictable loss of vision.
There are two main causes for failure in cases of retinal detachment surgery.
The first is that the body may make scar tissue in the eye. This scar tissue grows on the retina and also in the vitreous cavity. After a while the scar tissue shrinks and pulls the retina in toward the center of the eye. This form of scar tissue has a special name, proliferative vitreoretinopathy. Making scar tissue is a method used to heal wounds found in both plants and animals. It is a very basic response that has proven useful for millions of years. It is very difficult to stop scar tissue from forming.
The eye surgery for retinal detachment is a form of trauma itself and potentially can augment the tendency to form scar tissue. If proliferative vitreoretinopathy occurs the only option in trying to repair the eye is more surgery. If the scar tissue is removed from the eye, it can easily grow back. Fortunately scar tissue leading to redetachment is not that common and repeat surgery if it does occur is often successful.
The second main reason to have another detachment is a repeat of what caused the detachment in the first place. A second tear can form in the eye leading to another detachment. This will require additional surgery. It is often not possible to know if and when a second tear will form.
The sequence of events leading to a detachment are pulling by the vitreous to create a tear, fluid going under the retina to start the detachment process, and expansion of the detachment over time. In some patients the amount of time between the formation of the tear and complete retinal detachment can be a matter of hours. In other patients it may be many days.
If the tear is detected early, laser treatment to make welds can prevent progression of a detachment in many patients. The symptoms of retinal tears are not necessarily that different from that those experienced by patients having a simple vitreous separation.
If you have new or sudden flashes or floaters, darkness over part of your visual field, or a new loss of vision that does not go away, call your eye doctor or ophthalmologist right away. Floaters and flashes may be warning signs of retinal detachment.
There is no way to tell over the telephone if there are just simple floaters or a retinal tear. That is why examination by a retinal detachment doctor at our Retina Vitreous Center is necessary. If there is no retinal tear, well that was just a false alarm. If a retinal tear is present, then a ‘whole lotta hurt’ potentially could be saved by an in-office laser procedure.
Since the early clinical discovery, prevention, and selection of appropriate treatment are essential factors for the success rate for rhegmatogenous detachment repair, it is imperative to choose an expert in retinal detachment and tear repair.
Cutting-Edge Diagnostics. Early detection of retinal detachment or tear is crucial in order to preserve your eyesight. The best-in-class retinal detachment doctors at VRMNY use all types of ophthalmic imaging, including fluorescein angiography and indocyanine green angiography, as well as noninvasive imaging techniques like spectral domain optical coherence tomography, autofluorescence photography, and ultrasonography.
Newest Treatments. As leading experts in the treatment of retinal detachment, our retina detachment doctors research and develop new diagnostic and therapeutic strategies. Many current concepts in diagnosing and treating retinal detachment that are currently recognized worldwide are invented at the VRMNY. Our vitreoretinal surgeons provide surgical management of retinal detachment repair, including complex retinal detachments from diabetes and after trauma or failed primary repair.
World-class specialists. Our renowned retinal specialists lecture worldwide on retinal detachment treatments and serve as academic leaders in the field as the most published group in major peer-reviewed journals in the U.S. As nationally recognized experts, our physicians serve as reviewers for the premier journals, including the Archives of Ophthalmology, Ophthalmology, Investigative Ophthalmology, and Visual Sciences, Retina, Eye, and Graefe’s Archives of Clinical and Experimental Ophthalmology. Our doctors received several awards and have been granted permanent resident status in the United States as “outstanding scientists”.
Reputation. Our reputation for outstanding eye care gives you access to the latest retinal repair treatments and technologies and the best doctors for retinal detachment. Our specialists have been selected as Castle Connolly Top Doctors, New York Super Doctors, the prestigious group of New York Magazine Best Doctors, one of the best physicians in the United States by “The Best Doctors in America” and are consistently quoted by well-known retina specialists.
Do you want to learn more about retinal tear or detachment surgery in New York City? Please contact our office if you have any questions. Our top-rated retinal repair specialists are happy to assist you.
Let us help you enjoy your life
Call: (212) 861-9797To Speak With An Appointment Coordinator Now